11 Proven Ways to Support Homeless Individuals with Mental Health Needs in NY

The numbers are staggering – 101,978 people sleep in NYC shelters each night as of November 2025, and they desperately need mental health services. The situation becomes more alarming since 70 percent of shelter residents are families, with 34,393 children among them.
Finding shelter is just one piece of the puzzle. The statistics paint a sobering picture – about 30% of people facing chronic homelessness struggle with serious mental illness. Nearly two-thirds battle either substance use disorders or other chronic health conditions. These numbers highlight why targeted support makes such a difference.
Social workers, volunteers, and concerned citizens can create meaningful change by connecting vulnerable people with the right care. We outline 11 proven strategies to help homeless individuals with mental health needs and provides practical resources available throughout New York.
Mobile Mental Health Outreach Teams
Getting traditional healthcare seems impossible if you have both homelessness and mental health challenges. Mobile Mental Health Outreach Teams solve this problem by bringing vital services right to those who need them most.
Overview
Mobile Crisis Teams (MCTs) bring together behavioral health professionals who provide on-site mental health care to people in severe behavioral crises. The teams include master’s-level clinicians, social workers, peer specialists, and family peer advocates. Their main goal is to meet people “where they are,” both physically and emotionally.
These teams respond to calls between 8 a.m. and 8 p.m. and usually arrive within two hours. They aim to resolve crisis situations and provide help in comfortable environments. The teams work to avoid unnecessary police involvement or hospitalization while connecting people to ongoing care services.
MCTs have shown remarkable results. A study found that 55% of psychiatric emergencies handled by these teams were managed without hospitalization. Police intervention alone managed just 28% of similar cases. The teams also cut costs – cases handled by mobile crisis teams cost 23% less on average.
How Mobile Mental Health Outreach Teams support homeless individuals
People who experience homelessness face higher risks of behavioral health crises. The mechanisms behind this include health conditions, substance use, and specific life stressors. They often can’t access routine healthcare and deal with frequent police interactions.
These mobile teams help through:
- Face-to-face assessment and crisis intervention
- De-escalation techniques and harm-reduction strategies
- Short-term supportive counseling
- Connections to ongoing community-based mental health services
- Simple medical care including wound treatment
- Distribution of essential supplies (hygiene kits, food, water)
The numbers tell a powerful story – research shows that between 60-85% of individuals served by MCTs received help without going to jail or hospital. People who had stopped using mental health services are more likely to start again after meeting an MCT. This works especially well for those with depressive, mood, or psychotic disorders.
These teams do more than manage immediate crises. They help overcome common barriers like transportation problems, costs, and trust issues that keep homeless people from getting care.
Where to find Mobile Mental Health Outreach Teams in NY
New York City residents can request a Mobile Crisis Team by calling 988. The teams work in all five boroughs. Note that MCTs usually don’t work with people who are street homeless. HOMESTAT (Homeless Outreach Mobile Engagement & Street Action Teams) helps people living on the streets – just call 311.
S.H.O.W. (Street Health Outreach & Wellness) vans operate in these NYC neighborhoods:
- Elmhurst/Corona: Park of the Americas (Mondays)
- Jamaica: Union Hall Safe Haven (Thursdays)
- Lower East Side: Delancey Street (Monday through Friday)
- Midtown West: 39th Street between 8th and 9th Ave (Wednesday, Thursday)
The right service depends on the situation. Think over which option fits best – MCTs help people in shelters or temporary housing, while street outreach programs are better for those living outdoors.
Drop-In Centers with Mental Health Services
Drop-in centers are a vital lifeline that helps homeless individuals get immediate mental health support without the roadblocks they face with traditional services. These facilities bridge the gap between life on the streets and long-term solutions.
What Drop-In Centers offer
Drop-in centers differ from regular shelters. They provide detailed daytime services that meet immediate needs and connect visitors to long-term resources, while shelters mainly focus on overnight stays. Most centers give visitors essential services like hot meals, clean clothing, shower and laundry facilities, and a safe space indoors.
These centers also provide valuable support services:
- Case management and counseling services
- Help with job searches and benefit applications
- Mail and phone services
- Clean clothes and personal hygiene items
- Social activities
Many centers stay open 24/7—even during holidays—and are there when other services close down. This round-the-clock service becomes especially valuable at night, on weekends, and during holidays when regular mental health services take a break.
Mental health support at Drop-In Centers
Mental health services are the life-blood of what drop-in centers provide. These facilities take a non-clinical approach to mental health support in several ways:
Many centers provide professional mental health services that include psychiatric evaluations, counseling sessions, and links to medical care. They work with healthcare providers to give visitors their original assessments and connect them with ongoing treatment.
The centers stand out because they use a peer support model. People who have lived through mental health challenges often run or partner with these centers. This approach creates a space where visitors feel understood, not judged.
These centers put recovery and personal growth ahead of clinical treatment. One source puts it well: “At a drop-in center, there are people, not patients”. This mindset helps people who might have had bad experiences with traditional mental health systems feel more at ease asking for help.
Accessing Drop-In Centers in NYC
NYC has drop-in centers across all five boroughs, making help available whatever your location. Manhattan has four centers that never close: Mainchance, Olivieri Center, Paul’s Place, and 9th Avenue.
You’ll find other centers at:
- Bronx: The Living Room (800 Barretto Street)
- Brooklyn: Gathering Place (2402 Atlantic Avenue)
- Queens: QDIC (100-32 Atlantic Avenue) and Union Hall
- Staten Island: Project Hospitality (150 Richmond Terrace)
These centers welcome everyone, whatever their immigration status, and provide interpreters if English isn’t your first language. You don’t need an appointment—just walk in when you need help. The centers are near public transportation to make getting there easier.
Drop-in centers give people dealing with homelessness and mental health challenges a welcoming first step toward getting back on their feet.
Supportive Housing Programs
Supportive housing serves as the life-blood to tackle homelessness and mental health challenges at the same time. This innovative approach helps create lasting stability for people who find it hard to keep their housing while dealing with mental health conditions.
What is supportive housing?
Supportive housing combines affordable permanent housing with optional support services. These services help people who have experienced homelessness, stayed in hospitals, or faced incarceration. Unlike regular shelters, tenants get their own apartment or home. They also have access to detailed services that support their recovery and help them become part of the community.
Two main models exist:
- Single-site (congregate): Buildings where people have private living spaces but might share kitchens or common areas
- Scattered-site: Individual units spread across different neighborhoods and communities
The basic principle of supportive housing gives tenants the same rights as any other renter. They have the lease in their name and keep their housing whatever their participation in treatment programs. This “housing first” approach provides immediate, permanent housing without making treatment compliance or sobriety mandatory.
Mental health benefits of supportive housing
Research shows that supportive housing substantially improves outcomes for people with mental health challenges. Studies reveal that Housing First programs reduced homelessness by a median decrease of 89% compared to traditional approaches. About 86% of people with long histories of emergency room visits and arrests, along with substance use and severe mental illness diagnoses, successfully moved into and stayed in permanent supportive housing.
The mental health improvements go beyond stable housing. People living in supportive housing visit psychiatric emergency departments less often and use appropriate outpatient mental health services more. They report lower stress levels, less depression, and fewer mental health issues. This approach also results in better housing retention and more people taking part in mental health treatment.
Examples of supportive housing in NY
New York runs several strong supportive housing programs that help homeless people with mental health needs:
The NY/NY agreements provide supportive housing to homeless people with serious mental health conditions. NY/NY I and II require participants to be homeless and have a serious persistent mental health condition like Major Depression, Bipolar disorder, or Schizophrenia. NY/NY III needs people to be chronically homeless – meaning they must be homeless for at least one year out of the past two or two out of the past four years.
NYC’s 15/15 initiative helps four specific groups, including chronically homeless people with serious mental illness or substance use disorders. The Empire State Supportive Housing Initiative (ESSHI) helps families and individuals who are both homeless and have disabling conditions.
CAMBA provides supportive housing throughout Brooklyn with 873 units for both individuals and families. Their programs include special support for people who face substance use disorders and mental health challenges.
Street Psychiatry Initiatives
Street psychiatry brings professional mental health care right to homeless individuals. Mental health professionals meet people where they live – on park benches, under bridges, or in encampments. This innovative approach helps people who might never get care through traditional healthcare systems.
Understanding street psychiatry
Street psychiatry emerged about 20 years ago as a way to serve homeless populations with serious mental illness. Mental health teams follow the motto “Go to the people” and travel with backpacks full of medications, blood pressure cuffs, and other essential equipment.
Teams provide diagnostic assessments, manage medications, evaluate risks, and offer therapy in non-traditional settings. Street psychiatry wants to help people become stable enough to use clinic-based care and maybe even find housing.
How street psychiatry helps the homeless
The numbers tell a stark story – about half of all homeless people struggle with substance use disorders and/or serious mental illness. Life expectancy among homeless people is 30 years shorter than those who have homes.
Street psychiatry makes a difference through:
- Trust building with respectful, compassionate interaction
- Quick psychiatric assessments adapted to outdoor settings
- Medication prescriptions that work for street conditions
- Long-acting injectable medications instead of daily pills
- Links to broader healthcare and social services
Street psychiatrists know that homeless individuals need to stay alert for safety, so they don’t prescribe sedatives without clear permission. Treatment approaches adapt to each person’s living situation.
Programs offering street psychiatry in NY
New York runs several street psychiatry programs. Safe Options Support (SOS) Teams help homeless individuals with immediate needs while finding housing options. Licensed clinicians, care managers, and peer specialists work together in these teams that use the Critical Time Intervention model.
Janian Medical Care stands as NYC’s largest provider of psychiatric care to homeless individuals. Their street medicine teams work “park benches, underpasses and anywhere needed”.
Project Renewal’s mobile clinic parks outside Chelsea soup kitchen twice weekly. People can get psychiatric care without referrals, insurance, or prior diagnoses. Albany County launched a six-person street psychiatry team in 2023 with a nurse, mental health clinician, case manager, mental health advocate, substance abuse counselor, and supervisor.
NYC residents can access these services through SOS teams by emailing Coordinated Behavioral Care or calling 1-866-SOS-4NYC.
Peer Support and Recovery Programs
Peer support has emerged as a powerful tool in homeless mental health services. It builds on shared experiences rather than clinical expertise. The simple words “I’ve been there too” create an instant connection that traditional providers rarely achieve.
What are peer support programs?
Peer support programs employ individuals with lived experience of mental health challenges, substance use issues, or homelessness to help others in similar situations. These peers bring real-world understanding of recovery paths that clinical professionals might lack.
These programs take several forms:
- Intentional Peer Support (IPS) within organizations
- Peer-led self-help and mutual support groups
- One-on-one recovery mentorship
- Online peer-to-peer interactions
Peer supporters take on multiple roles. They offer emotional support, provide practical help, and share their recovery stories to show that positive change is possible.
Benefits of peer-led mental health support
Research strongly backs peer interventions. Studies reveal that peer support improves quality of life among vulnerable populations. It also reduces hospital visits during mental health crises.
Peer support brings unique advantages:
- Builds trust and rapport through shared experiences
- Cuts down self-stigma while building hope
- Helps people connect better with community services
- Shows that recovery can happen
- Saves money for health systems
The benefits reach peer supporters too. Many report stronger self-confidence and better self-image from sharing their stories.
A recipient shared this experience: “I was depressed, angry, and hostile in the shelter. The peer staff were friendly and showed concern in helping me find an apartment. I feel more relaxed when speaking with them each week. This helped me be positive, and I achieved my goal of getting an apartment”.
Where to find peer support in NY
New York organizations provide peer support specifically for homeless individuals with mental health needs.
The Safe Options Support (SOS) program includes peers in their teams to build understanding and inspire hope. RiseWell runs peer outreach services with recovery specialists who support people moving from hospitals back into community life.
Veterans experiencing homelessness benefit from the HUD-VASH program. Those who interact more often with peer specialists show better housing stability.
Despite cultural barriers and funding challenges, peer support grows stronger across New York as a vital part of complete homeless mental health services.
Integrated Health and Shelter Services
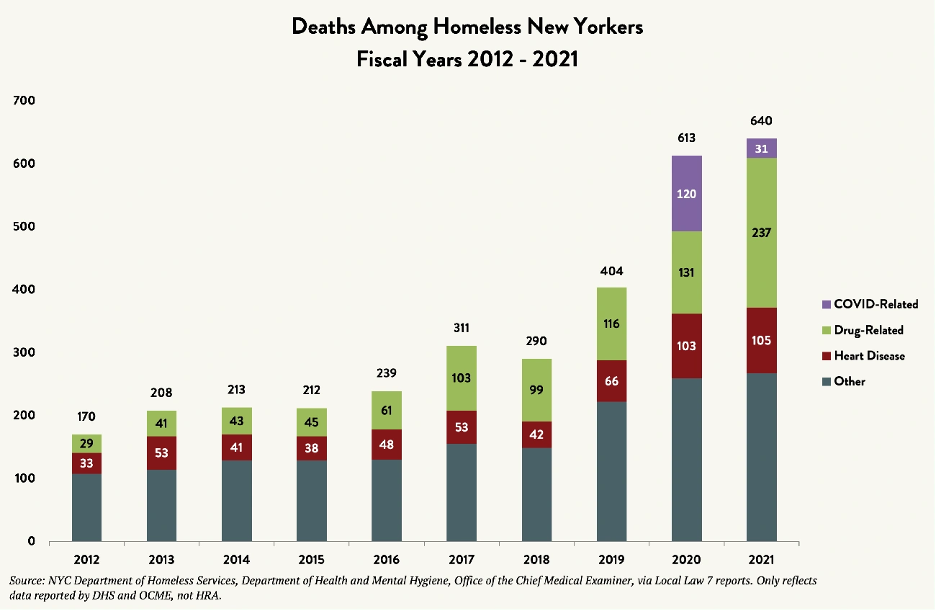
Image Source: Coalition For The Homeless
Mental health services combined with housing solutions work best to help homeless people who face psychological challenges.
Combining shelter and mental health care
Mental health care and shelter services work together to give detailed support that helps with immediate housing needs and mental health conditions. Care for the Homeless (CFH) shows this approach through their Patient-Centered Medical Home model that offers integrated primary care and behavioral health services at 15 sites across NYC. These integrated facilities provide psychiatric services, mental health counseling, substance abuse treatment, and specialized support for conditions like HIV.
Examples of integrated service models
Susan’s Place stands as a remarkable example—a 200-bed transitional residence built for homeless women with mental illness or medical frailty. The facility has helped more than 1,000 women find permanent housing since opening in 2008. Bridge to Home offers another innovative solution that helps people who leave hospitals with ongoing psychiatric challenges but don’t qualify for extended hospital stays. Healthcare professionals, including psychiatric providers and peer specialists, staff this program 24/7. They provide detailed care with medication management, therapy, and substance use disorder treatment.
The Safe Options Support (SOS) program uses the Critical Time Intervention model to connect street homeless individuals with housing while providing person-centered care. Project Hospitality has created a chain of compassionate care that combines clinical services with various housing options—emergency, transitional, and permanent supportive.
How to access these homeless resources
The ICL Hope Center can provide immediate help at 844-ICL-HOPE (844-425-4673). Their trained staff will connect you to suitable programs. You can access SOS services by emailing Coordinated Behavioral Care or calling 1-866-SOS-4NYC. The Urban Pathways 9th Avenue and Olivieri Drop-in Centers stay open 24/7 and provide meals, clothing, showers, and connections to mental health resources.
Legal Aid for Mental Health Advocacy
Legal problems make mental health issues worse for people experiencing homelessness. These individuals struggle to navigate complex legal systems while managing their mental wellbeing without proper support.
Legal challenges faced by homeless individuals
People with mental health disabilities run into legal obstacles about housing, income maintenance, and government benefits. These challenges include:
- Unwarranted evictions and housing discrimination
- Difficulty accessing entitled benefits
- Civil rights violations through criminalization
- Barriers to healthcare access
The Supreme Court’s Grants Pass decision reversed previous protections against penalizing unhoused people for sleeping in public spaces. The situation has become more concerning recently. People with mental health conditions who are homeless face involuntary commitment more often now—a process that uses homelessness itself as proof of potential danger.
How legal aid supports mental health
Legal assistance is a vital shield against declining mental health. The stress of legal battles can make mental health conditions worse, lead to hospital stays, and end up causing homelessness.
Attorneys help stop this downward spiral through early legal help. A team approach works best when lawyers work with mental health providers. This prevents people from losing their income or housing when their mental health gets worse.
Research shows real results: Veterans who got full legal representation had major improvements within three months. Their symptoms of hostility, paranoia, psychosis, anxiety disorders, and PTSD decreased substantially. People who met their legal goals showed better outcomes in housing status and community integration.
Organizations offering legal aid in NY
Mobilization for Justice helps adults with mental health disabilities throughout NYC with civil legal matters. Contact: 212-417-3700
The Legal Aid Society’s Homeless Rights Project defends homeless families’ rights and serves as counsel to the Coalition for the Homeless. They defended the right to shelter when NYC tried to change eligibility requirements recently.
Urban Justice Center’s Mental Health Project helps with housing matters and benefits access. Their criminal justice work fights against treating mental illness as a crime. Contact: found on their website
If you need immediate help with mental health-related legal issues in Central NY, call (877) 777-6152.
Trauma-Informed Care Training for Providers
Trauma-informed care marks a transformation in healthcare providers’ approach to homeless people with mental health needs. Homeless populations often carry extensive trauma histories, making proper training essential for service providers to help effectively.
What is trauma-informed care?
Trauma-informed care (TIC) creates a service delivery framework that acknowledges and responds to trauma’s widespread effects. This approach changes the basic question “What’s wrong with you?” to a more compassionate “What happened to you?”.
TIC has four key elements:
- Service providers’ awareness of trauma
- Focus on physical and emotional safety
- Ways for clients to rebuild control
- A strengths-based approach that builds on resilience
Six core principles form the foundation: safety; trustworthiness and transparency; peer support; collaboration and mutuality; giving people voice and choice; and cultural, historical, and gender considerations.
Why it matters for homeless mental health
Research shows traumatized individuals face major hurdles to finding stable housing. Trauma creates barriers that make it hard to use available services and can slow development, especially for people without stable homes.
Trauma-informed methods help prevent re-traumatization in clinical settings. This approach goes beyond providing resources – it helps providers respond to psychological and emotional needs with empathy rather than blame.
Training programs available in NY
New York offers several trauma-informed care training options:
Project Renewal provides complete, trauma-informed medical and mental health services throughout NYC. The Coordinated Care Services Inc. (CCSI) runs a six-session trauma-responsive practice program. This program covers basic concepts, neurobiology, equity, healing, compassion resilience, and hope.
The National Health Care for the Homeless Council has created a three-part training package that specifically addresses homelessness and traumatic stress. Trauma-Informed NY helps connect providers with training resources across the state.
Access to Addiction and Detox Services
Breaking the cycle of homelessness and addiction needs special programs that tackle both problems at once.
Link between addiction and homelessness
Addiction and homelessness are deeply connected. About 30% of people who face long-term homelessness have serious mental health issues, and roughly two-thirds deal with substance use disorders or other lasting health conditions. Studies show that 20-35% of homeless people struggle with substance abuse.
The cause-and-effect relationship isn’t clear cut. Some people lose their homes because of substance abuse that destroys relationships and drains finances. Others start using drugs or alcohol after they become homeless to cope with life on the streets. Living without stable housing puts constant pressure on people and often pushes them toward more drug use and drinking.
Mental health support in detox programs
Good treatment programs know that about half the people with mental health issues also face substance abuse, which doctors call “co-occurring disorders”. These programs go beyond basic detox and offer:
- Treatment plans built around each person’s needs
- Recovery plans that work on both problems
- Safe housing during treatment
This blended approach helps people recover better from both substance use and mental health issues, and their lives improve overall.
Where to find addiction services in NY
New York State has several organizations that help homeless people with addiction:
The Office of Addiction Services and Supports (OASAS) puts money into permanent housing programs that help homeless people with substance use disorders. Monroe County has many community groups that provide outpatient care, rehab, and residential treatment with fees based on what people can pay. Care for the Homeless (CFH) offers medical and mental health services, including addiction counseling, at many locations across the city.
Employment and Job Training with Mental Health Support
A stable job is the life-blood of mental health treatment for homeless people. A meaningful job does more than provide money – it gives people purpose and connection that can revolutionize their recovery.
How jobs affect mental health
The numbers paint a grim picture. Almost 90% of people with serious mental health issues don’t have jobs. This number jumps to 96% for homeless individuals battling mental illness. People stuck in this cycle of unemployment face worse stress, anxiety, and depression. They also struggle to get the care they need.
Regular work improves both physical and mental health. People with jobs rely less on emergency shelters and find it easier to escape homelessness. Work also helps them build social connections that are crucial for long-term recovery.
Programs offering job training and counseling
These organizations step up to fill this vital need:
- Postgraduate Center for Mental Health gives full assessments, job training, placement help, and career advice
- Housing Works runs Ready For Work (RFW)—an 8-week program that blends classroom learning with internships. Workers can earn bonuses: $500 when they get hired, $500 after 30 days, and $1,000 after 90 days
- The Guidance Center provides job services including training and coaching
Examples of successful initiatives in NY
Project Renewal’s Next Step Employment Program helps people prepare for and land living-wage jobs. They also offer training in food services and organic farm-to-table sales. Urban Pathways uses the proven Individual Placement and Support model, which works well for people with serious mental illness. Brooklyn Clubhouse gives people temporary work for 12-20 hours each week over 6-9 months. This helps them build skills and resumes at their own pace.
Community-Based Mental Health Clinics
Community mental health clinics are a lifeline that brings neighborhood-focused care right to homeless people who need it most.
Role of community clinics in mental health
Community clinics act as first responders for homeless people facing mental health challenges. Many clinicians work beyond office settings and provide services in their client’s familiar surroundings like homes or public spaces. These clinics help with psychiatric evaluations, medication management, and counseling through licensed social workers, psychiatrists, and psychiatric nurse practitioners. They focus on recovery through person-centered care that values meaningful relationships over clinical transactions.
Accessibility for homeless individuals
These clinics remove major barriers to care. They don’t require health insurance cards—a common roadblock that keeps people from getting help. The wait times are much shorter—just minutes instead of hours or days at regular facilities. Location matters too—having health services near where homeless people live makes it easier for them to get care.
Examples of clinics offering homeless resources
The Institute for Community Living (ICL) gives detailed services to New Yorkers with serious mental illness and substance use disorders. NYU Langone’s Community Medicine Program sends mental health professionals straight to homeless shelters. Janian Medical Care—NYC’s largest provider of psychiatric care for homeless people—places clinicians in 40 supportive housing residences across the city. Health Care for the Homeless provides free services whatever your insurance or immigration status.
Next Steps
Helping homeless people with mental health needs takes more than just one approach. This piece shows eleven tested ways to help vulnerable New Yorkers live better lives.
These resources work best together. Mobile outreach teams link people to drop-in centers and supportive housing, while peer support specialists share their experiences to give others hope. Street psychiatry brings care right to those who can’t or won’t use regular services.
The numbers tell a harsh story—almost 102,000 people sleep in NYC shelters each night, and many face mental health issues. But New York’s complete network of services gives real paths to stability and recovery.
You can help those in need as a social worker, volunteer, family member, or concerned citizen. Just knowing where to send someone can start their path to healing.
Each homeless person has their own story and needs. Getting them the right care might seem tough at first, but these specialized programs offer expert help and support.
Get to know the local resources in your borough. You could start by volunteering at a drop-in center or reaching out to your local mobile crisis team. Small actions create big changes—pointing someone to the right program could save their life.
Tackling homelessness and mental health issues isn’t easy. All the same, your understanding and knowledge of available resources can help New York’s most vulnerable people get better.
